Many Consumers Have Delayed Healthcare Appointments
We are well over a year into living with COVID-19 infiltrating all corners of the globe. We have all likely come due for at least an annual preventive health screening and one or two dental cleanings. For some of us in the US, going to the doctor’s office has been seen as an unnecessary risk. While the ability to have a virtual or telehealth visit has helped many continue with their care, according to a recent Big Village Caravan survey, a sizable portion of those in the US have delayed or missed getting care as a result of the pandemic.
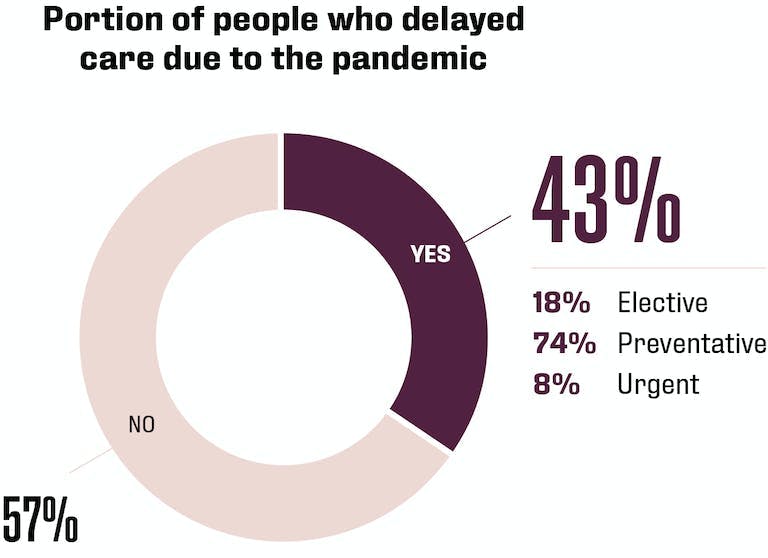
- Elective care was missed or postponed less often by seniors (65+, 9%) compared to younger and middle-aged individuals (18 – 44, 62%).
- Men (42%) and black patients (8%) were less likely to postpone or delay preventive care compared to women (58%) and non-Hispanic whites or Hispanics (64% and 20% respectively).
- Health status (i.e. self-reported as healthy or unhealthy) did not play a role in choosing to delay or miss care.
Big Village’s recent results (data collected in March 2021) may indicate a promising behavioral shift in more recent months as compared to the initial six months of the pandemic. During the early months, the Robert Wood Johnson Foundation and the Urban Institute conducted studies which showed a troubling effect of health status on delayed care. Understandably, a greater portion of higher risk individuals (56% suffering from chronic or multiple conditions) delayed care in comparison to about 25% of those not suffering from a physical or mental health condition, chronic illness or multiple conditions.[1]
However, our results may be a reflection of self-reported health status. In other words, it is possible that patients with a physical or a mental health condition would not describe themselves as unhealthy. This may be especially true if their condition is under control or being well managed. .
Trouble Scheduling Healthcare Appointments
Access to care has also been an issue due to the pandemic. Among the 30% of US residents who experienced scheduling difficulties, a few disparities were observed by Big Village including:
- Hispanic patients reporting greater difficulty scheduling than non-Hispanic white patients (59% vs 21%).
- Those with children in the household also encountered more challenges compared to childless or empty nest households (53% vs 47%).
- Those in urban locations experienced more issues than those in rural areas (38% vs 19%).
- Employed individuals struggled more often than retirees (67% had difficulty vs 13%).
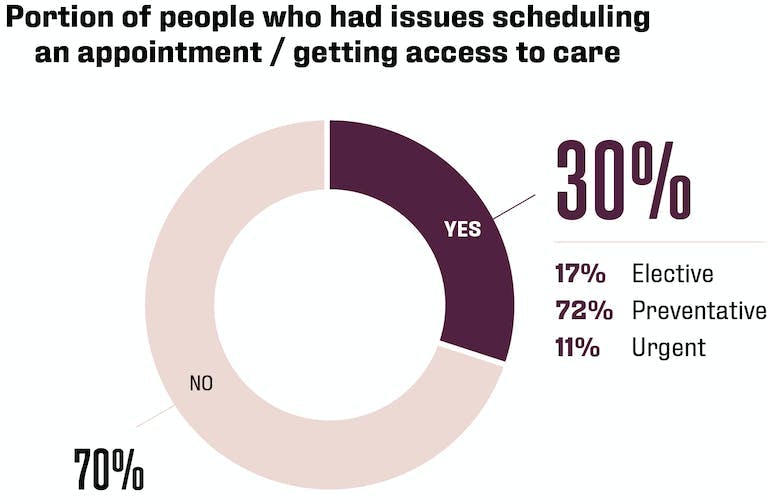
With the reduction in elective procedures and backlog for preventive care, getting an appointment tends to be easier for those with more flexibility in their schedule when it comes to elective procedures. More specifically, 56% of patients aged 18 – 44 experienced an issue compared to 24% of those aged 55+ (more likely to be empty nesters and/or retired).
As with delays and missed appointments, the recent Big Village Caravan survey did not show self-reported health status as a factor in greater ease or difficulty for scheduling care. Preventive care scheduling issues were more often experienced by employed individuals compared to retirees (63% vs 17%). Urgent care access issues were experienced significantly more often by younger patients (age 18 – 44, 69%) than seniors (65+, 3%).
Overall, it is promising that the majority of patients still sought care and have not had difficulty getting the care that they need. Additionally, for those who did chose to delay care or who experienced difficulties scheduling care, they are more likely to be going without elective procedures or preventive routine care rather than more pressing medical needs. Only three percent avoided or mentioned difficulty receiving urgent care. As patients become more comfortable seeking preventive care, it is possible that access will become more difficult for these visits as the backlog catches up to routine care that has not been skipped or postponed.
As my colleague Margaret Rorick mentioned in an earlier blog, Health and the Pandemic, many people reported positive behavior changes over the past year. While the majority of US consumers maintained their exercise rates, healthy eating, alcohol consumption and smoking habits, a portion hovering around 30% reported positive shifts in behavior while between 10% and 25% changed their behaviors in a potentially harmful way.
Behavioral Changes Positive, Negative and Neutral During the Pandemic
| Behavior | Increased Behavior | Behaved as Always | Decreased Activity |
| Drinking alcohol | 14% 👎︎ | 52% | 34% 👍 |
| Snacking between meals | 36% 👎︎ | 53% | 10% 👍 |
| Smoking | 10% 👎︎ | 51% | 38% 👍 |
| Exercising | 28% 👍 | 47% | 25% 👎︎ |
| Seeking mental health care | 20% 👍 | 58% | 22% 👎︎ |
| Sleeping well | 23% 👍 | 54% | 24% 👎︎ |
| Eating healthy foods | 33% 👍 | 54% | 13% 👎︎ |
| Meditating | 24% 👍 | 58% | 19% 👎︎ |
Legend: 👎︎ = Negative Behavior, 👍 = Positive Behavior
Most people plan to keep their behaviors the same after the pandemic is over. For those who made positive changes, this may mean continuing with their new behaviors at the same rate as they practiced them during the pandemic. For those who did not change behaviors during the pandemic, remaining consistent regardless is the case for most Americans. A notable portion of individuals plan to increase positive behaviors and decrease negative behaviors post pandemic. With the exception of increased snacking between meals, fewer than one-in-ten Americans plan to increase potentially harmful behaviors or decrease positive behaviors.
Anticipated Behavior Post Pandemic Positive, Negative and Neutral
| Behavior | Will Increase Post Pandemic | Will Remain the Same Post Pandemic | Will Decrease Post Pandemic |
| Drinking alcohol | 8% 👎︎ | 58% | 34% 👍 |
| Snacking between meals | 16% 👎︎ | 59% | 25% 👍 |
| Smoking | 6% 👎︎ | 54% | 41% 👍 |
| Exercising | 44% 👍 | 50% | 6% 👎︎ |
| Seeking mental health care | 19% 👍 | 61% | 20% 👎︎ |
| Sleeping well | 31% 👍 | 61% | 8% 👎︎ |
| Eating healthy foods | 41% 👍 | 54% | 5% 👎︎ |
| Meditating | 22% 👍 | 61% | 17% 👎︎ |
Legend: 👎︎ = Negative Behavior, 👍 = Positive Behavior
Supporting Positive Change in Consumer Behavior
A commonly held belief is that it takes 80 days or 80 repetitions to form a habit. While we have been living with COVID-19 for more than 80 days, are the changes that we’ve adopted likely to stay as we get busier? We may have good intentions but what can we do to keep reinforcing our healthy habits? Here are a few suggestions to keep up the progress we have made as individuals and as a society:
- Schedule the dental and/or preventive care visits that were skipped or that are due.
- Make a plan for how you can continue to eat healthy if returning to work in an office. Considering weekend meal prep to avoid those trips to the hamburger line in the cafeteria or the fast-causal restaurant around the corner.
- Continue to take breaks throughout your day, meditating for 10 – 15 minutes, taking a short walk, or performing light yoga can help energize you and make you more productive.
- Make time for healthy habits – getting regular exercise and enough sleep. Make it a priority or habit to work out at the same time each day and to turn off the TV, put down the phone and turn off the laptop at a set time every day to ensure you remain well rested.
- Stay connected to how you are feeling and recognize when it is time to step back. Burnout is real and has been a prominently discussed topic over the past year, let’s not lose the ground that has been gained in fighting the urge to wear burnout as a badge of honor.
- Employers need to continue acknowledging employee physical and emotional health and maintain environments that provide support and encourage growth.
- Employers can also continue promoting an open dialog around safety concerns and be supportive of alternative working arrangements. Many healthy behavior changes are likely to have been possible due to the lessened amount of time commuting which may have contributed to a greater sense of work life balance without compromising productivity.
- Physicians and insurance providers can continue to reach out to members of high-risk populations for both physical and mental health aliments.
Pandemic or not it is important to remember that everyone is silently fighting their own personal battles each day. Let’s not forget what we have learned and make a habit of continuing to be respectful of everyone and their unique needs/life situation. The kindness and empathy that we have embraced during the pandemic can and should continue.
Big Village regularly partners with health care providers, insurers, and organizations across a diverse array of industries to measure expectations of customers, members, patients, and employees relative to experience. Organizations that will remain strong and secure the greatest loyalty will continue along the path of empathy and support. Organizations that are willing to invest in understanding the needs of their key stakeholders (customers, patients, members and employees) and commit to continuously evolving their products, offers, services and policies to fit their unique needs, will see the greatest return on their investment.
Whether your current situation is a lack of customer, patient, employee or member input or lack of action to reform problematic processes, Big Village is the perfect partner to work with regardless of your current state of customer experience measurement and maturity. We meet our clients where they are and help them evolve at a pace conducive to their unique needs and corporate culture. Let us know how we can help.
Written by Nicole Garberg, VP of Customer Experience at Big Village Insights.
[1] https://patientengagementhit.com/news/a-third-of-adults-skip-healthcare-access-during-covid-19s-first-act